Acute Lymphoblastic Leukemia Treatment
There are several different ways to treat adult ALL patients.
Some treatments are standard (currently used), and some new treatments are undergoing clinical trials. A clinical trial is a research study whose goal is to improve the standard treatment method or to obtain information about the results of new treatments for cancer patients. If clinical trials show that the new treatment is better than the standard, the new treatment can subsequently become the standard treatment. Patients may also participate in clinical trials. In some clinical trials, only patients who have not received any treatment may participate.
Treatment of adult acute lymphoblastic leukemia usually takes place in two stages.
Stages of treatment of adult acute lymphoblastic leukemia:
- Remission-induction therapy. The goal of this stage of treatment is to destroy leukemia cells in the blood and bone marrow and achieve remission.
- Post-remission therapy. This is the second stage of treatment. It begins as soon as remission is achieved. The goal of post-remission therapy is to destroy the remaining leukemia cells, which may not be active, but can subsequently begin to grow and this will lead to relapse. This stage is also called the continuation of remission therapy.
Treatment and prophylactic therapy of the central nervous system is usually carried out at each stage of treatment. Due to the fact that chemotherapeutic drugs are taken orally or injected intravenously, the drug often can not destroy the leukemia cells that enter the central nervous system (brain and spinal cord). Leukemic cells take refuge (hide) in the central nervous system. Intrathecal chemotherapy and radiation therapy can destroy leukemia cells that have fallen into the central nervous system, and thereby prevent a relapse of the disease. This type of treatment is called treatment and prophylactic therapy of the central nervous system.
Today, there are four standard methods of treatment:
Chemotherapy
Chemotherapy is a method of treating cancer with potent chemotherapeutic drugs. Chemotherapeutic drugs can stop and destroy the growth of cancer cells, prevent their separation and penetration into other tissues and organs. With chemotherapy, medications can be taken orally (in the form of tablets, capsules) or injected intravenously or intramuscularly. The drug enters the bloodstream, spreads throughout the body and infects cancer cells (systematic chemotherapy). If chemotherapeutic drugs are injected directly into the spine (intrathecal chemotherapy), an organ or cavity (e.g., abdominal), the drug mainly affects cancer cells in these areas (regional chemotherapy). Combination chemotherapy is a treatment in which more than one anti-cancer chemotherapeutic drug is used. The way chemotherapy is used depends on the type and stage of the cancer.
Intrathecal chemotherapy can be used to treat adult ALL, which tends to spread to the brain and spinal cord. Therapy used to prevent the spread of cancer cells in the body and their penetration into the brain or spinal cord is called treatment and prophylactic therapy of the central nervous system. Intrathecal chemotherapy is carried out in combination with conventional chemotherapy, in which medications are taken orally or by injection.
Intrathecal chemotherapy
Antineoplastic agents are injected into the intrathecal cavity of the spinal canal, where cerebrospinal fluid is located (CSF is shown in blue in the figure). There are two different ways to administer chemotherapy drugs. The first method, depicted at the top of the figure, is a drug administered in an Ommaya reservoir. (A convex container that is inserted into the ventricles of the brain. The container holds the bulk of the drug so that the drug can slowly enter the brain through small tubes). Another method, shown at the bottom of the figure, is the drug injected directly into the cerebrospinal fluid into the spinal column at the level of the lower back. The procedure is carried out under local anesthesia.
Radiation therapy
Radiation therapy is a cancer treatment method that uses hard X-rays or other types of radiation to kill cancer cells or prevent the growth of cancer cells. There are two types of radiation therapy. External radiation therapy – a special device focuses radiation in the tumor area. Radiation internal therapy – the use of radioactive substances hermetically sealed in needles, capsules, rods or catheters, which are placed directly in or near the tumor. External radiation therapy can be used to treat adult ALL, which tends to spread to the brain and spinal cord. This is called treatment and prophylactic therapy of the central nervous system.
Chemotherapy followed by stem cell transplantation
Chemotherapy is performed before stem cell transplantation. Stem cell transplantation is used to replace abnormal blood-forming cells with full ones. Stem cells (immature blood cells) are taken from the blood or bone marrow of a patient or donor, frozen and stored. At the end of the chemotherapy course, the stored stem cells are thawed and administered to the patient in the form of stem cell infusions. Transplanted stem cells take root and help restore bone marrow cells producing blood cells.
Tyrosine Kinase Inhibitor Therapy
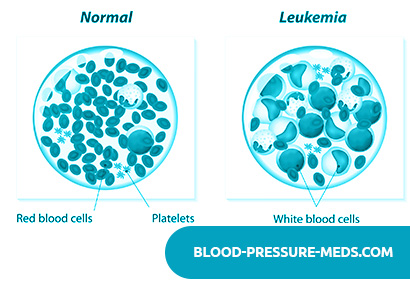
Anticancer drugs called tyrosine kinase inhibitors are used to treat certain types of adult ALL. The drug blocks an enzyme, tyrosine kinase, which promotes the development of a large number of white blood cells (granulocytes or blast cells) from stem cells. To date, two such drugs, Imatinib (imatinib mesylate) (Gleevec) and Dasatinib, are used.
Some new treatments are undergoing clinical trials.
This section describes the types of treatments that are in clinical trials. It is impossible to talk about all the new treatments that are being studied. Clinical trial information is available on the NCI website.
Biological therapy
Biological therapy is a treatment method that uses the patient’s immune system to fight cancer. Substances that are produced in the body or that are synthesized in the laboratory are used to stimulate or restore the natural mechanisms of protection and the fight against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
Patients may also participate in clinical trials.
For some patients, participating in clinical trials is the best choice. Clinical trials are part of the research process. The purpose of conducting clinical trials is to establish: whether the new treatment is safe and effective, or better than the standard treatment.
Many of the current standard treatments are based on early clinical trials. Patients participating in clinical trials may receive standard treatment or undergo a new treatment regimen.
Patients who take part in clinical trials contribute a lot to research and help improve the way they treat cancer in the future. Even if the results of clinical trials do not indicate the effectiveness of the new treatment method, but they often provide answers to very important questions and help to take the research one step further.
Patients may participate in clinical trials before, during, and after they have begun treatment.
In some clinical trials, only patients who have not received any treatment may participate. Patients in whom the disease is not treatable can also participate in clinical trials. There are also clinical trials that are exploring new ways to prevent relapse or eliminate side effects that result from cancer treatment.
Re-examination
Some tests that were done to diagnose cancer or the stage or form of the disease can be repeated. Sometimes the tests are repeated to monitor the effectiveness of the treatment. The decision to continue, change, or discontinue treatment is based on the results of these tests.
Some tests need to be done from time to time and after treatment. The results of the tests can show a change in the patient’s condition or the presence of a relapse of the disease. Sometimes such analyzes are called control.
Prevention of Acute Lymphoblastic Leukemia
A dose of 24 grams per head is given for 3 weeks at 1.5 grams per session from two lateral fields.
One of two injections of methotrexate, administered 2 times a week into the spinal canal, during head irradiation is advisable to be done on Saturday, as there is usually no radiation therapy on this day, and the other on one of the first days of the week. After a session of irradiation of the head; on the day of the endolumbar administration of methotrexate, the patient remains in the hospital.
During the prevention of neuroleukemia using both irradiation and the administration of methotrexate and cytosar, patients receive 6-mercaptopurine daily at a dose of 25 mg / m2 and cyclophosphamide at a dose of 100 mg / m2 once a week.
After the end of the prophylaxis of neuroleukemia, bone marrow puncture is performed, and if there are no signs of relapse, then maintenance therapy is started.
The second method for the prevention of neuroleukemia is the endolumbar administration of methotrexate and cytosar. Drugs are administered with an interval of 3-4 days, with poor tolerance once a week.
Both methods of prevention of neuroleukemia are reliable and allow you to abandon the supporting intralumbal administration of methotrexate.
Continuous maintenance treatment during the period of improvement of acute lymphoblastic and undifferentiated leukemia of children is carried out on an outpatient basis, for 5 years until complete improvement. They begin treatment immediately after achieving full improvement or after courses consolidating the achieved improvement.
Children receive continuous treatment with three drugs according to the following scheme: 6-mercaptopurine orally daily; methotrexate inside on the 6th day of the week; cyclophosphamide inside on the 7th day of the week, these days 6-mercaptopurine is not canceled.
For the “risk group” during the period of continuous maintenance treatment with three drugs every 1.5-2 months, a course of AR AR is performed. During this course, within a week after it, maintenance treatment with three drugs is canceled, and then during the week is carried out in half doses. After that, maintenance treatment is carried out in full doses.
Continuous treatment conditions:
1) a blood test with the determination of platelets and reticulocytes 1 time per week;
2) with a decrease in the level of leukocytes to 1 H 103 – 2 H 103 (1000-2000) in 1 μl, the doctor halves the dose of cytostatic drugs, with a subsequent increase of more than 2.5 H 103 (2500) in 1 μl, restore the previous dose;
3) treatment is interrupted at any stage when the level of leukocytes in the blood falls below 1000 in 1 μl, with a significant increase in temperature, stomatitis, diarrhea;
4) a bone marrow puncture in the first year of improvement is performed 1 time per month; on the 2-5th year of improvement – 1 time in 3 months.
The treatment of acute lymphoblastic leukemia is enhanced when it comes to the process of T-cell nature. According to the program of American pediatric oncologists, to eliminate the manifestations of the disease in T-lymphoblastic acute leukemia, they begin with intravenous administration of cyclophosphamide at 1200 mg / m2 on the 1st day of treatment or between the 2nd and 5th day (with a leukocyte level of more than 5 × 104 (50,000) in 1 μl and significant organomegaly requiring prior administration of allopurinol due to the high level of uric acid in serum and the risk of developing uric acid diathesis). From the 3-4th day (or on the 1st day, if cyclophosphamide administration is delayed) weekly (1 time per week), according to this program, as well as according to the Aur program, vincristine is administered for 4 weeks, and prednisolone and rubomycin are also used in doses and in terms corresponding to Scheme 2 of treatment of acute lymphoblastic leukemia.
When remission is achieved, a course of its consolidation is carried out, including 5-day continuous administration of cytosar 100 mg / (m2 / day), thioguanine (or 6-mercaptopurine) 50 mg / m2 every 12 hours for 5 days of cytosar administration. Conduct 3 courses of treatment with cytosar and thioguanine (6-mercaptopurine) with an interval between courses of 14 days.
Then, within 7-14 days, L-acnapaginase is administered dropwise at 200-300 U / kg. In the case of a high level of leukocytes and a large mass of tumor lymph nodes of splenomegaly or hepatomegaly, therapy should be carried out by prescribing a large amount of liquid, alkaline drink, along with allopurinol for the prevention of uric acid diathesis.
If with T-cell acute leukemia in the mediastinum, enlarged lymph nodes are determined, which are poorly contracted by chemotherapy, then local irradiation of this area at a dose of 30 Gy is recommended; local radiation is also advisable with a significant increase in the lymph nodes of any other area.
Treatment during the improvement period with T-cell leukemia should be enhanced: along with continuous therapy with 6-mercaptopurine, methotrexate, cyclophosphamide.